- Dr. Oubre's Digest
- Posts
- Bad coding causing bad metrics?
Bad coding causing bad metrics?
And why that matters to physicians.

Starting TODAY, get a 7 day free trial of our CDI and Coding Village online community! This offer ends February 25!
Next webinar:
Story time:
A group of gastroenterologists felt their GI bleed average length of stay was higher than they expected. When they reviewed the charts, they suggested many were coded wrong.
A group of cardiologists felt their heart failure readmission rates were higher than they expected. When they reviewed the charts, they suggested many were coded wrong.
A 3rd party vendor emailed some members of hospital administration suggesting that when a patient’s hospitalization is extended due to something that developed after admission, we should recode it to that diagnosis.
Spoiler: They weren’t coded wrong and that 3rd point is absolutely wrong.
Why? Because those people didn’t understand the selection of the principal diagnoses… which is okay. Physicians and administrators aren’t supposed to be coders (but please consult your coding team before jumping to conclusions).
What is the principal diagnosis?
I suggest any administrator or physician who tracks clinical metrics understand it. It’s addressed on page 106 of the Official ICD-10-CM guidelines.
The principal diagnosis is “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care.”
“The admission” are the keywords here.
Why?
Because a condition that is not present at the time of admission cannot be coded as the principal diagnosis. They say it’s what “bought the bed.” Now that you know that simple coding 101 fact, you know why that 3rd point above was wrong.
Also, when two conditions are both present at the time of admission, that condition which requires more resources may be chosen as the principal diagnosis.
Why does principal diagnosis matter?
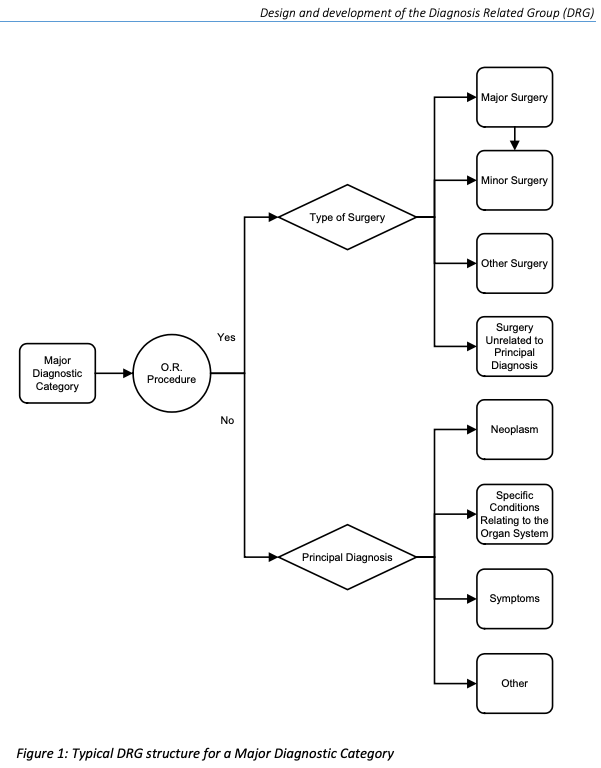
The principal diagnosis determines the DRG (except when a procedure is performed, then the procedure typically drives the DRG). I explained DRGs in a previous newsletter.
That’s important because many physicians track their metrics based on DRG, and MANY different codes “map to” that DRG.
Misconception Examples
Let’s go back to the gastroenterologists. They decided to have their metrics tracked by the typical DRG for GI bleeds with EGDs (DRGs 326 - 328).
The problem? Though they were doing their jobs well and scoping those patients within 24 hours, they were often staying in the hospital longer due to other issues such as heart failure or waiting for skilled nursing facility placement. But, those circumstances would not change the principal diagnosis and ultimate DRG assignment.
Why? Again:
A procedure would be considered “more resources” than some IV lasix.
Often the heart failure exacerbation was not present at the time of admission.
So, the GI bleed DRG was assigned every time (appropriately).
Speaking of heart failure, let’s talk about those cardiologists and their heart failure readmission rates. Ignoring some CMS oddities that I won’t bore you with, they had a different issue: dreaded combo codes and sequencing rules!
Another basic coding 101 fact? Coding assumes a relationship between some conditions such as:
Hypertension and heart involvement
Hypertension and kidney involvement
Even if you don’t say they’re linked, coding assumes they are (they will not be linked if you specifically document that they are not). Moreso, sequencing rules will often require that these combo codes get coded first (often resulting in the principal diagnosis).
How did that impact our cardiologists?
Patients were coming in with things like complications from their hypertension and chronic kidney disease. Their heart failure was chronic, stable, not in exacerbation, and not a main focus of care.
But because of the combo codes and sequencing rules?
BAM.
It was included in the principal diagnosis and mapped to the DRG by which they were being tracked.
Does it make clinical sense?
Not really.
Was it coded wrong?
Nope.
My suggestions to physicians
Understand how your metrics are tracked! Do not agree to metrics that determine your pay without fully understanding them. Demand that your lead coder is in the room when negotiating with your administration, or ask them lots of questions after the meetings. Use your CDI and coding teams as resources.

Consider having your metrics tracked by the principal diagnosis codes themselves, rather than DRG (therefore avoiding the “wide net” that DRGs cast). This is how the CMS AMI 30-day readmission cohort is tracked, which I discussed in a previous newsletter.
And, of course, complete and accurate documentation is key.
Ensure documentation is clear about what was present on admission, and what was not.
Make sure documentation is clear about the main underlying etiology of symptoms.
Give a final diagnosis by the time of discharge (e.g. Chest pain vs GERD vs ACS. Acute right MCA infarct versus “neurological symptoms.”)
Know that coding is complex and confusing. It often doesn’t make sense clinically (and that’s not coders’ fault, they have to follow the guidelines). Coders go through lots of schooling and it takes YEARS of experience to get it right. Sure, it’s good to question things, but don’t jump to conclusions. And know that your health system routinely audits coders to ensure their accuracy.
Don’t miss out on a 7 day free trial of our CDI and Coding Village online community (offer expires Feb 25)!
That’s all for now. Don’t hesitate to ask questions as they help inspire future issues!
Cheers,
Robert
Thanks to fellow villagers Laura Samson, RN CCDS, Kelli Scardino, RHIT CCS, Penny Jefferson, RN CCDS, Alicia Whiteford, RN CCDS, and Revka Stearns, CCS CPC for their contributions to this newsletter!
When you’re ready, there are 3 ways I can help you:
Join our CDI and Coding Village online community! It’s impossible to know it all, it takes a village! What you’ll get:
Learn from me and other experienced professionals (perfect for new coders / CDI’s and those pivoting their career)
Participate in monthly interactive webinars hosted by me, weekly 1 minute CDI quick tip videos, and anatomy and physiology reviews not found anywhere else
Share ideas & solutions to new problems with peers in real-time discussions
Check out The Practical Guide to Attending Documentation video course.
Stop underbilling your hard work & MASTER the new billing rules
Get 3.5 hours of CME credit! (Use your CME funds!)
Stop feeling guilty about writing shorter notes
Use notes to PREVENT getting sued
Check out The Resident Guide to Clinical Documentation video course. The course that helps you:
Impress your attendings and improve your evaluations.
Prepare for real-world productivity pressures
Gain the confidence to write shorter yet more effective notes.
Use notes to make you a better, more prepared physician
If you were forwarded this newsletter and would like to subscribe:

Reply