- Dr. Oubre's Digest
- Posts
- SOFA-2 Update
SOFA-2 Update
The changes, why they matter, and clarifying misunderstandings

I tried keeping this newsletter as concise as possible. For a complete review of the SOFA-2 update (with a surprise guest), check out my webinar in my online community. If you’re confused by anything below, I likely addressed it in the webinar.
After 30 years, the long awaited update to SOFA is here (as was suggested in the 2016 Sepsis-3 definition publication).
Published October 29, 2025 in JAMA, it’s already the hot topic amongst clinicians, CDI specialists, and revenue cycle professionals.
But with that comes misunderstandings and miscommunications. So, let me address the biggest one off the bat:
This is not a new sepsis definition
The sepsis-3 definition is “Life-threatening organ dysfunction due to a dysregulated host response to infection.”
That has not changed.
In the sepsis-3 publication, the SOFA score was used to describe “life threatening organ dysfunction” given it’s ease of use, familiarity to the clinical community, and it’s validated association with mortality.
However, the sepsis-3 article also says, “Neither qSOFA nor SOFA is intended to be a stand-alone definition of sepsis.”
But given their association, it’s understandable why some consider this a “new sepsis definition.” We must caution ourselves, both clinically and in the revenue cycle, from completely marrying the two as there are certainly evidence-based non-SOFA sepsis-related organ dysfunction - especially as health plans use additional restrictions on top of SOFA to issue clinical validation denials. To that end, based on comments from the lead author Dr. Mervyn Singer (who was also an author of the Sepsis-3 definition), it seems the authors are aware of how health plans have been weaponizing SOFA in denials (more on this later).
SOFA Score Changes:
Brain (renamed from “central nervous system”)
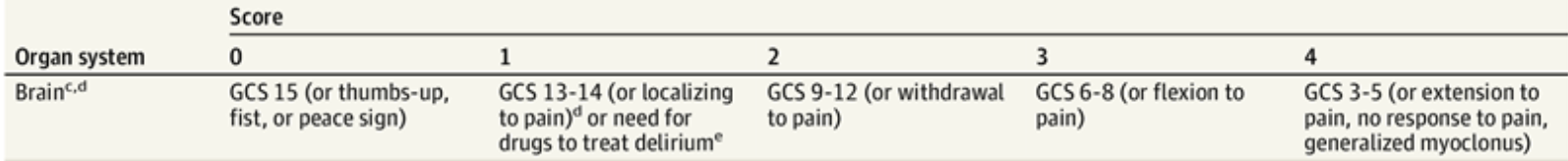
1 point:
GCS score of 13 – 14 (unchanged from SOFA-1)
If drugs are used to treat delirium even if GCS score is 15. They reference drugs included in the “International management of pain, agitation, and delirium in adult patients in the ICU guidelines” but I cannot find any publication with that name (nor in their references). Perhaps it is the Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU which is published in a Q/A format. The main medications mentioned are Precedex and Haloperidol. In my opinion, that seems incomplete as other medications such as risperidone, olanzapine and quetiapine are often used… especially as the caption includes “long term use” of medications for delirium. I’d like to see some clarification on that.
They do now include additional descriptors such as localizing pain (see picture) which I like because health plans have started to deny if no GCS is documented. Internists and intensivists are much more likely to document these descriptors versus GCS.
2 points
GCS 9 - 12 (or withdrawal to pain) (SOFA-1 was 10 - 12)
3 points
GCS 6 - 8 (or flexion to pain) (SOFA-1 was 6 - 9)
4 points
GCS 3 - 5 (or extension to pain, no response to pain, generalized myoclonus) (same as SOFA-1 with addition of pain/myoclonus descriptors)
Respiratory
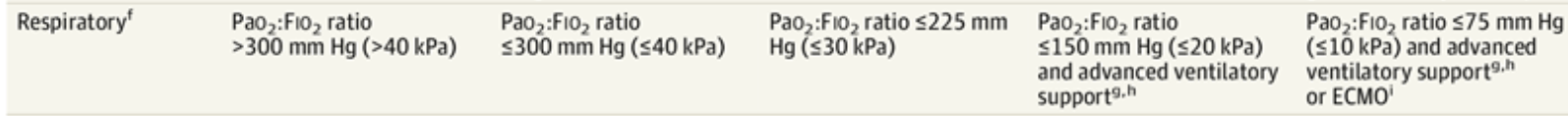
1st column is 0 points
The thresholds are generally higher (meaning lower numbers) for P:F ratio compared to SOFA-1. However, they have now included an alternative SpO2:FiO2 ratio when P:F ratio (i.e. an ABG) is not available. Caveat: SpO2 must be less than 98%. This should be a win for denial appeals as health plans give no credence to S:F ratio despite evidence suggesting it’s adequate.
1 point
P:F ratio <300 (previously 400);
OR S:F ratio <300
2 points
P:F ratio <225 (previously 300);
OR S:F ratio <250
3 points
P:F ratio <150 (previously 200);
OR S:F ratio <200 (must be receiving advanced ventilatory support)
4 points
P:F ratio <75 (previously 100);
OR S:F ratio <120 (must be receiving advanced ventilatory support or ECMO)
The max amount of points someone NOT receiving advanced ventilatory support is 2 unless not using because the devices are not available or due to “ceiling of treatment” (which was a phrase I was not familiar with - this is essentially when higher forms of treatment are not used due to provider/family decision such as goals of care).
Advanced ventilatory support is defined as receiving high-flow nasal cannula, CPAP, BiPAP, noninvasive ventilation, invasive mechanical ventilation, or long-term home ventilation.
The use of ECMO should be assigned 4 points for the respiratory component only when being used for respiratory indications. However, when ECMO is being used for a cardiovascular indication, 4 points should be assigned for both the cardiovascular and respiratory components.
Abridge transforms clinical conversations into complete, accurate notes, helping physicians spend less time documenting and focus more on patient care. In a recent ROI analysis with partner health systems, clinicians reported spending up to 23% less time documenting, and observed meaningful improvements in RVUs per encounter—driven by more complete and accurate documentation.
Cardiovascular
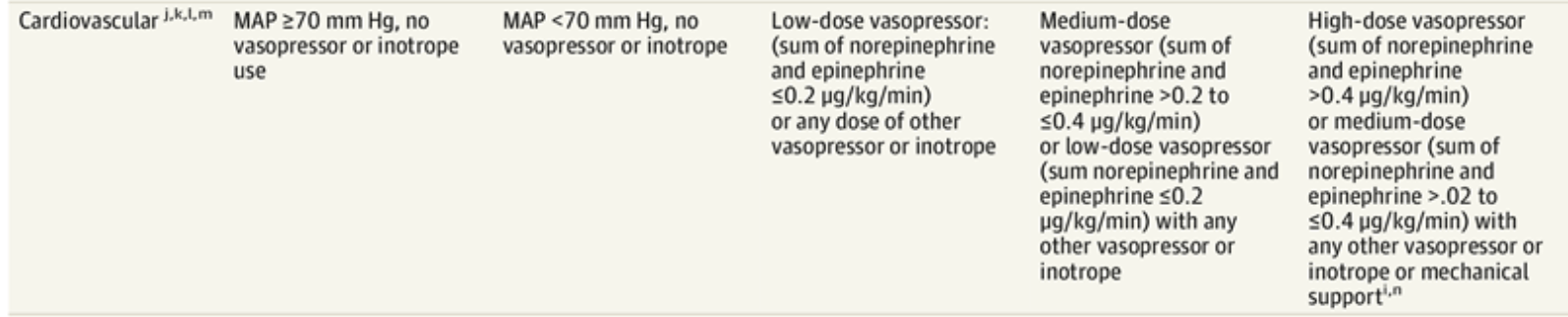
1st column is 0 points
The cardiovascular component still centers on mean arterial pressure and vasopressor use, but SOFA-2 offers more nuance and was updated for modern vasopressor use.
1 point
MAP <70 aka 60 - 69 (unchanged)
2 points
Low dose vasopressor: Sum of norepinephrine and epinephrine <0.2 ug/kg/min OR any dose of other vasopressor or inotrope;
OR dopamine <20 ug/kg/min;
OR MAP 50 – 59 (if vasopressors are not being used due to “treatment ceiling”)
3 points
Medium dose vasopressor: Sum of norepinephrine and epinephrine >0.2 to <0.4 ug/kg/min;
OR low-dose vasopressor (sum of norepinephrine and epinephrine <0.2 ug/kg/min) with any other vasopressor or inotrope;
OR dopamine >20 - <40 ug/kg/min;
OR MAP 40 – 49 (if vasopressors are not being used due to “treatment ceiling”)
4 points
High-dose vasopressor: sum of norepinephrine and epinephrine >0.4 ug/kg/min;
OR medium-dose vasopressor (as detailed above) wth any other vasopressor or inotrope or mechanical support;
OR Dopamine >40 ug/kg/min;
OR MAP <40 (if vasopressors are not being used due to “treatment ceiling”)
Liver
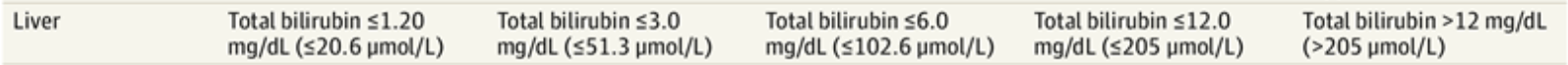
1st column is 0 points
The liver thresholds are tweaked slightly but the basic pattern is unchanged.
1 point
Bilirubin 1.21 - <3.0 (SOFA-1 range was 1.2 - 1.9)
2 points
Bilirubin 3.1 - <6.0 (SOFA-1 range was 2.0 - 5.9)
3 points
Bilirubin 6.1 - <12.0 (similar to SOFA-1)
4 points
Bilirubin >12 (similar to SOFA-1)
Kidney (renamed from “renal”)
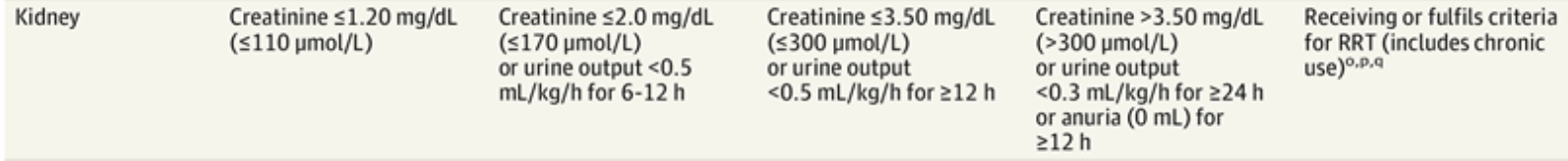
1st column is 0 points
1 point
Cr 1.21 - <2.0
OR UOP <0.5 ml/kg/hr for 6 - 12 hours
2 points
Cr 2.1 - <3.5
OR UOP <0.5 mk/kg/hr for >12 hours
3 points
Cr >3.5
OR UOP <0.3 ml/kg/hr for >24 hr
OR anuria (0 mL UOP) for >12 hr
4 points
Receiving or fulfils criteria for renal replacement therapy (RRT aka dialysis) (includes chronic use);
OR if RRT is not used due to "ceiling of treatment" and they otherwise meet criteria: Cr >1.2 or <0.3 ml/kg/hr UOP for >6 hr and at least one of the following:
Potassium >6.0
OR pH <7.2 with bicarb <12
The article did not expand on what they mean by "includes chronic use" for renal replacement therapy. Does that mean patients on chronic dialysis automatically get 4 points? I’m not entirely sure. If someone has clarity on that, please let me know.
Note that receiving RRT for non-renal causes (such as for intoxications, hyperkalemia for other reasons, acidosis for other reasons, Uremia for other reasons, etc.) does not get you 4 points in the kidney category.
If receiving intermittent RRT, score 4 points on days not receiving RRT until RRT is terminated.
Hemostasis (renamed from “coagulation”)

1st column is 0 points
The platelet thresholds changed slightly:
1 point
Platelets <150 (same as SOFA-1)
2 points
Platelets <100 (same as SOFA-1)
3 points
Platelets <80 (SOFA-1 was 50)
4 points
Platelets <50 (SOFA-1 was 20)
What the paper says about fluids
Nothing.
Literally, the words “fluids,” “bolus,” and “hydration” are not mentioned anywhere in the publication.
I point this out as health plans are routinely requiring that SOFA criteria be met “after IVF bolus” or “after adequate hydration.” The authors could easily have endorsed that approach if they agreed with it.
They did not.
Again, based on comments from the lead author, it seems clear they knew how health plans have been misusing SOFA, and I suspect the wording in this update reflects that.
How the score is actually calculated
The 1st bullet point under the SOFA-2 score table is this: “The final score is obtained by summing the maximum points from each of the 6 organ systems individually within a 24 hour period.” This is an important clarification as health plans commonly issue denials based on:
Taking the lessor of the scores
Only those that were obtained at the same time
Only those that were obtained on the same day (but the article says that for missing data after day 1 of ICU care, carry forward the last observation - the rationale being that non measurement suggests stability)
And, again, only those which were obtained after fluids. This strategy directly contradicts SOFA-2.
Closing thoughts
Is SOFA-2 more restrictive than SOFA-1? Yes, slightly. For total SOFA score, more patients had lower values in SOFA-2. When the authors reclassified patients from SOFA-1 to SOFA-2, they found that 49% of the time, their SOFA scores remained the same. 11% of the time, their SOFA-2 score was higher. 40% of the time, their SOFA score was lower.
With that said, I believe the new SOFA-2 score helps us on the denial appeals side with added nuance.
As health plans react to SOFA 2, expect to see new denial language that tries to spin this paper in their favor and/or combines requirements from Sepsis-3, SOFA-1, and SOFA-2. Make sure to highlight the points I’ve mentioned above, and read the paper in its entirety to make sure you understand it yourself (only about a 15 minute read). Print it out. Bring a pen and highlighter.
If you want even more information about SOFA-2, check out my webinar in our online community with a 7-day free trial - you’ll also get 14 hours of recorded webinars hosted by me and other experts, complete PDF summaries on top CDI topics, weekly case reviews, my exclusive CDI tip card, direct access to me, and access to our forums (with >400 topics and growing) where you can share ideas & solutions to new problems with peers in real-time discussions!
Share your thoughts in the comments, or on Linkedin!
That’s all for now. Cheers,
Robert
Thank you to Laura Samson, RN BSN CCDS for editing this newsletter!
Check out what other subscribers are enjoying:
Our CDI and Coding Village online community. Join with a 7-day free trial! It’s impossible to know it all, it takes a village! What you’ll get:
>14 hours of recorded webinars hosted by me and other experts
Complete PDF summaries of top CDI topics
Weekly case reviews
My exclusive CDI Tip card
Access to our forums (with >400 topics and growing) where you can share ideas & solutions to new problems with peers in real-time discussions!
Direct access to me
Cover your cost (and then some) with our affiliate and village advisor programs!
The Practical Guide to Attending Documentation video course.
Write shorter notes and get home faster with 100% confidence you’re billing appropriately.
Get 3.5 hours of CME credit! (Use your CME funds!)
Use notes to protect yourself from lawsuits
The Resident Guide to Clinical Documentation video course. The course that interns and residents:
Impress your attendings and improve your evaluations.
Prepare for real-world productivity pressures.
Gain the confidence to write shorter yet more effective notes.
Use notes as a checklist to prevent mistakes and provide more complete care.
If you were forwarded this newsletter and would like to subscribe:
If you were forwarded this newsletter and would like to subscribe:


Reply